Inflammation, pain, and restricted mobility – the trio that defines arthritis, a complex spectrum of conditions affecting millions worldwide.
Learn about arthritis, including osteoarthritis, rheumatoid arthritis, fibromyalgia, gout, and systemic lupus erythematosus (SLE). Discover the changeable and non-modifiable elements that influence it, as well as the usual therapies that give relief. Beyond medications, embark on a journey into the realms of physical activity and diet, discovering how they intersect with arthritis management. Unearth the power of nutrition, learning about foods that support joint health and those that contribute to inflammation. Continue reading and navigate the vast landscape of it, empowering yourself with knowledge to navigate this intricate terrain.
What is Arthritis?
Arthritis is a condition that refers to inflammation in the joints, where bones meet in one or more places on the body. It is derived from the Greek word arthron (meaning “joint”) and the Latin word itis (meaning “inflammation”).
While “arthritis” is usually thought to be a single disease, it really refers to a group of over 100 medical diseases marked by inflammation or discomfort in muscles, joints, or surrounding fibrous tissue, sometimes known as rheumatism or rheumatic conditions. These disorders have a cumulative effect on the musculoskeletal system, producing stiffness and discomfort around joints. Some, such as lupus and rheumatoid arthritis, may affect internal organs and the immune system.
The Centers for Disease Control and Prevention (CDC) reported that a 2013 survey revealed approximately 52.5 million U.S. adults had physician-diagnosed arthritis in 2010-2012, representing over 1 in 5 adults. This marked an increase of 2.5 million from 2007 to 2009, aligning with projections estimating a staggering 67 million American adults living with arthritis by 2030, as per the National Health Interview Survey (NHIS).
What Causes Arthritis and Who is Affected?
While arthritis is commonly associated with aging, affecting a larger proportion of adults, it is not exclusive to this demographic—individuals of all ages, including children, can be diagnosed with various forms of arthritis.
Given the broad classification of conditions under arthritis, the causes, and manifestations vary significantly. However, a shared characteristic among them is the presence of inflammation or pain in muscles, joints, or fibrous tissue surrounding the joints.
Let’s delve into a more detailed exploration of five prevalent forms of arthritis:
- Osteoarthritis
- Rheumatoid arthritis
- Fibromyalgia
- Lupus
- Gout
1. Osteoarthritis
Impacting around 27 million adults in the United States, osteoarthritis stands as the predominant type of arthritis diagnosed in America. This condition arises when the cartilage, a crucial cushioning tissue at the ends of bones within joints, undergoes breakdown and erosion. 1
As the smooth cartilage surface diminishes, losing its ability to act as a shock absorber during bone movement, it becomes thinner and rougher. In severe cases, osteoarthritis can lead to the complete wearing away of cartilage, resulting in constant bone-on-bone friction.
Manifesting as pain, inflammation, and potential mobility restrictions, osteoarthritis often induces a deep aching sensation in and around the affected joints. Stiffness may be experienced after prolonged periods of sitting or upon waking. Swelling in one or more joints, along with the sensation or sound of bones rubbing or crunching, is also characteristic of osteoarthritis.
Commonly affecting weight-bearing joints like knees, hips, and ankles, osteoarthritis may also target joints in the feet, hands, and cervical spine. Its development is typically linked to factors such as injury, infection, or the natural aging process. Additionally, a family history of the disease may elevate the risk of osteoarthritis.
2. Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a progressive inflammatory ailment that wreaks havoc on organs and joint tissues. Stemming from an immune system malfunction—ordinarily the body’s defender against harmful organisms—RA redirects its attack towards the membrane lining the joints. This assault on the synovial membrane, the soft tissue nestled between the joint capsule and cavity, can result in the erosion of both bone and cartilage within the joints. The consequence: pain, swelling, and the potential for deformity and disability if left unaddressed.
Diverging from osteoarthritis, RA is classified as an autoimmune disease. This classification denotes a type of arthritis where the immune system turns against the body’s own tissues. Consequently, RA extends its impact beyond joints, affecting areas like the eyes, mouth, and lungs. While RA can target any joint, the wrists and fingers are commonly affected.
Symptoms linked with rheumatoid arthritis encompass joint swelling, tenderness, and warmth, stiffness, fatigue, joint pain, fever, and diminished joint function.
The precise triggers for rheumatoid arthritis in certain individuals remain unclear. However, there is a belief that a combination of genes, environment, and hormones contributes to the risk of developing this form of arthritis. It notably affects women more frequently than men and typically emerges in individuals aged 35 to 60, although it can strike older individuals and even children. 2
3. Fibromyalgia
Fibromyalgia, also known as fibromyositis or fibrositis, is a complex and chronic pain disorder characterized by persistent fatigue and musculoskeletal pain that extends across joints, tendons, muscles, and various soft tissues throughout the entire body. Derived from “fibro” (fibrous tissue like ligaments and tendons), “my” (muscles), and “algia” (pain), the term encapsulates the essence of this sometimes incapacitating form of arthritis.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) notes that approximately 5 million people aged 18 or older in the United States grapple with fibromyalgia. Despite its prevalence, fibromyalgia is labeled as a syndrome, not a disease, as it lacks a definitive cause, identifiable signs, or symptoms. Often referred to as the “Great Imitator,” it presents diverse symptoms and severity levels, with manifestations unique to each individual.
Widespread pain is a shared experience for those with fibromyalgia, encompassing sharp shooting pains, deep aches, and muscle twitches. Tender points in specific areas, including the back of the neck, shoulders, chest, elbows, hips, buttocks, lower back, shins, and knees, exhibit pain or tenderness when pressure is applied. Additional symptoms include chronic fatigue, stiffness, temporomandibular joint dysfunction, tingling, or numbness in hands and feet, sleep disturbances, impaired concentration (typically termed “fibro fog”), dizziness, balance issues, and chronic headaches, including migraines.
While the definitive cause of fibromyalgia remains elusive, it typically emerges following physical trauma, such as surgery, acute illness, or accidents. Trauma affecting the central nervous system is believed to act as a catalyst. Genetic factors may contribute to susceptibility, with a gender discrepancy—more women than men are diagnosed.
About 80 percent of fibromyalgia patients are female, primarily in their childbearing years, ranging from 20 to 50 years old. While diagnoses occur in men of similar ages and elderly individuals, they are less frequent. Although rare, fibromyalgia can also impact children. 3
4. Systemic Lupus Erythematosus (SLE)
Systemic lupus erythematosus, a variant of arthritis and an autoimmune disease, represents the most prevalent form of lupus, often referred to simply as “lupus.” In individuals with SLE, the immune system deviates from its protective role, attacking healthy cells and tissues instead of safeguarding the body against harmful organisms. This autoimmune response impacts every organ system, causing diverse effects depending on the individual. SLE can inflict damage on joints, skin, blood vessels, heart, lungs, kidneys, and the brain.
Typically, individuals with systemic lupus erythematosus endure symptoms such as profound fatigue, joint pain or swelling, muscle aches, skin rashes, unexplained fevers, discoloration in fingers or toes, anemia, blood-clotting complications, mouth ulcers, swollen glands, dizziness, and headaches. SLE is characterized by alternating periods of illness and remission. 4
While the precise causes of SLE remain elusive, connections to genetics, environmental factors, and hormones are considered. Unlike other autoimmune diseases, SLE is not linked to a specific gene, but individuals with lupus often have family members with autoimmune conditions. While lupus can affect anyone, it predominantly occurs in women, with a higher prevalence among women of African American, Native American, Hispanic, and Asian descent. 5
5. Gout
A prevalent and painful manifestation of arthritis, gout impacts approximately 3 million adults in the United States. 6
This condition arises when uric acid accumulates in the body, stemming from the breakdown of purines found in body tissues and certain foods like dried beans, peas, liver, and anchovies. Ordinarily, uric acid dissolves in the blood, passes through the kidneys, and is excreted in urine. However, when this process falters and uric acid accumulates, it crystallizes into needle-like formations, causing severe joint pain and potentially leading to kidney stones.
Gout often initiates its assault on the big toe, inducing sudden burning pain, stiffness, and swelling. It can also target joints in the ankles, heels, knees, wrists, fingers, and elbows. Without effective control, gout attacks can recur and, over time, inflict damage on joints, tendons, and other tissues.
Factors influencing the risk of developing gout include genetics, gender, and weight. A family history of gout increases the likelihood of an individual developing it, and men are more predisposed than women. While gout can affect people of any age, it predominantly emerges in adults. Overweight individuals face an elevated risk due to increased tissue breakdown, leading to excess uric acid production. Additionally, consuming purine-rich foods like anchovies, asparagus, dried beans, mackerel, mushrooms, sardines, and scallops can exacerbate gout.
Risk Factors
Given the vast array of over 100 different types of arthritis, the factors influencing the development of these conditions vary considerably. Nevertheless, certain risk factors have been consistently linked to an elevated likelihood of arthritis onset. These risks fall into two categories:
- Modifiable, where proactive measures can be taken to effect change, and
- Non-modifiable, representing factors beyond alteration.
Modifiable Risk Factors
Excessive Weight or Obesity: Surplus weight is a contributing factor to both the initiation and advancement of the majority of arthritis types.
Prior Joint Injuries: Previous damage or injury to a joint may play a role in the genesis of arthritis in that particular area.
Infection: Body infections have the potential to trigger the development of various types of arthritis.
Non-Modifiable Risk Factors
Arthritis often occurs alongside other chronic health conditions, with approximately half (47%) of U.S. adults with arthritis reporting at least one additional ailment. Notably, more than half of individuals with heart disease (57%) or diabetes (52%), and over one-third with high blood pressure (44%) or obesity (36%), also struggle with arthritis. 10
- Age: The likelihood of developing most forms of arthritis escalates with advancing age.
- Gender: Women are more commonly affected by the majority of arthritis types, constituting about 60% of all diagnosed cases. Gout, however, is more prevalent in men.
- Genetics: A familial history of arthritis heightens the risk of developing certain forms of arthritis. Genetics also play a role in elevating the risk factors for specific autoimmune disorders such as rheumatoid arthritis and systemic lupus erythematosus.
Common Arthritis Treatments
The medications prescribed for arthritis management vary depending on the specific type of arthritis. Below are some commonly utilized medications for arthritis patients:
Corticosteroids: Including prednisone and cortisone, corticosteroids aid in reducing inflammation and suppressing the immune system. They can be administered orally or injected directly into the affected joint.
Disease-Modifying Antirheumatic Drugs (DMARDs): Predominantly used in treating rheumatoid arthritis, DMARDs work by slowing or halting the immune system’s attack on the joints. Methotrexate (Trexall) and hydroxychloroquine (Plaquenil) are two examples.
Analgesics: Aimed at pain reduction without addressing inflammation, analgesics include acetaminophen (e.g., Tylenol), tramadol (e.g., Ultram or Ryzolt), and narcotics containing hydrocodone (e.g., Vicodin or Lortab) or oxycodone (e.g., Percocet or Oxycontin).
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These drugs alleviate both pain and inflammation. Over-the-counter NSAIDs like ibuprofen (e.g., Advil or Motrin IB) and naproxen (e.g., Aleve) are common, while certain NSAIDs are available only with a prescription. Some NSAIDs also come in cream or gel forms for direct application on joints.
Physical Activity and Diet to Manage Arthritis
Arthritis manifests differently in individuals, making a one-size-fits-all cure for its associated pain and symptoms elusive, given the multitude of arthritis forms. Treatment strategies are influenced by factors such as the duration and severity of the illness. The primary focus of arthritis treatment lies in alleviating symptoms and enhancing joint function.
Physical activity emerges as a widely encouraged treatment for various arthritis types. Exercises can enhance range of motion and bolster the muscles surrounding joints. The effectiveness of exercise depends on the specific arthritis form and the extent of bodily damage. Medical professionals emphasize the potential harm of inactivity for most arthritis patients. Without regular physical activity, muscles weaken, joints stiffen, balance issues intensify, and pain tolerance diminishes. Inactivity also heightens the risks of cardiovascular disease and type 2 diabetes. Physically active arthritis patients typically enjoy improved health, experiencing enhancements in pain management, sleep quality, energy levels, and daily functioning.
Dr. David Borenstein, President of the American College of Rheumatology and a practicing rheumatologist, underscores, “Many people with arthritis and rheumatic diseases suffer from joint pain and stiffness, which can cause a person to avoid exercise out of the fear of increasing their pain or causing injury. However, exercise, when properly planned and safely executed, can do just the opposite.”
In addition to physical activity, maintaining a well-balanced diet is crucial for naturally and effectively managing arthritis. Optimal food choices not only provide essential nutrients but also support the maintenance or attainment of a healthy body weight. Excess weight exerts additional pressure on weight-bearing joints, exacerbating arthritis symptoms. Many arthritis sufferers find that even a modest weight loss positively impacts their quality of life.
Foods to Incorporate into a Nutrient-Rich Diet for Arthritis
For individuals managing arthritis, adopting a diet rich in fruits, vegetables, fish, nuts, legumes, and olive oil is beneficial. Additionally, restricting or avoiding red meat, saturated fats, dairy, and sugar can aid in arthritis prevention and contribute to inflammation and pain management.
Omega-3 Fatty Acids
Scientific studies suggest that omega-3 fatty acids possess anti-inflammatory properties, potentially mitigating arthritis symptoms. These acids work by suppressing the production of enzymes that erode cartilage. Foods rich in omega-3s include oily fish and fish oil supplements, with top choices being salmon (wild, fresh, or canned), herring, sardines, rainbow trout, Pacific oysters, flaxseeds (ground and oil), chia seeds, and walnuts.
Cruciferous Vegetables
According to research from the Mayo Clinic, cruciferous vegetables like broccoli and cauliflower demonstrate protective effects against arthritis development. Other recommended options include cabbage, Brussels sprouts, kale, and bok choy.
Vitamin D
Increased dietary vitamin D intake is associated with a reduced risk of certain arthritis types. Opt for sources like oily fish (tuna, mackerel, cod, and sea bass) and exposure to sunlight, the natural source of vitamin D.
Olive Oil
Diets rich in olive oil, such as the Mediterranean style, have demonstrated pain and stiffness reduction in arthritis individuals. Olive oil’s anti-inflammatory properties, attributed to oleic acid, polyphenols, and omega-3 fatty acids, make it a preferred choice. Extra virgin olive oil, with the highest antioxidant content, is recommended.
Ginger
Acknowledged for its anti-inflammatory and antioxidant properties, ginger can be incorporated into meals by adding sliced ginger to tea, grating fresh ginger over sautéed vegetables, or sprinkling ground ginger in batters. Note that ginger acts as a blood thinner, potentially interacting with blood-thinning medications.
Vitamin C
Essential for collagen health, vitamin C is a major component of cartilage. Increased vitamin C intake is linked to a reduced risk of certain arthritis forms. Opt for dietary sources like bell peppers, oranges, guava, mangoes, grapefruits, strawberries, pineapple, broccoli, cauliflower, and kidney beans, avoiding high-dose vitamin C supplements that may worsen arthritis symptoms.
Anthocyanidins
Powerful antioxidants found in foods like cherries, blackberries, raspberries, strawberries, grapes, and eggplant, anthocyanidins may help reduce inflammation associated with arthritis, according to a Harvard School of Public Health study.
Green Tea
Containing the antioxidant epigallocatechin-3-gallate (EGCG), green tea may help prevent the production of inflammatory chemicals involved in arthritis. Preliminary research suggests that EGCG and other catechins in tea may preserve joints longer.
Carotenes
Carotenoids, powerful antioxidants in fruits and vegetables, include beta carotene (found in pumpkin, carrots, kale, butternut squash, cantaloupe, sweet potatoes, and spinach) and beta-cryptoxanthin. The latter may decrease the risk of inflammation-related conditions like arthritis. Foods rich in beta cryptoxanthin include winter squash, pumpkin, persimmons, papaya, tangerines, sweet peppers, corn, collard greens, oranges, and apricots.
Natural Sources of Vitamin
Natural Sources of Vitamin B12
- Clams
- Salmon
- Haddock
- Trout
Natural Sources of Vitamin A
- Yellow vegetables (summer squash)
- Carrots
- Green leafy vegetables (kale, spinach, greens, and romaine lettuce)
- Fruits (cantaloupe, tomatoes, and apricots)
Natural Sources of Vitamin D
- Tuna
- Liver oils
- Mackerel
- Cod
- Sea bass
Natural Sources of Calcium
- Plain low-fat yogurt
- Sardines
- Salmon
- Seafood with bones
- Turnip greens
- Spinach
- Kale
- Broccoli
- Nuts (almonds, Brazil nuts, and pecans)
Restrict or Eliminate These Pro-Inflammatory Foods
Trans Fats
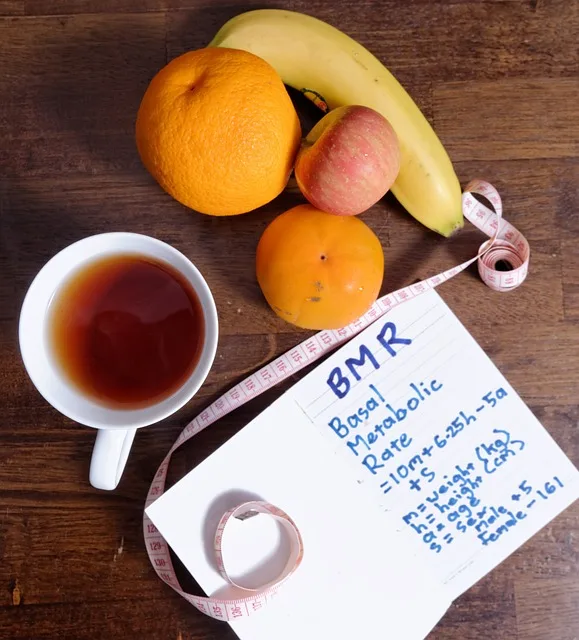
Also known as hydrogenated oils, trans fats are artificially created in factories to extend the shelf life of food. This process solidifies vegetable oils by adding hydrogen, raising LDL (low-density lipoprotein) cholesterol levels (known as “bad cholesterol”) and elevating the risk of inflammation, heart disease, and other health issues. Common sources of trans fats include packaged and processed snack foods, crackers, cookies, certain margarine, shortening, fried foods, and baked goods like pastries, biscuits, and pizza dough.
Saturated Fats
Primarily found in animal products like dairy (ice cream, butter, whole or 2 percent milk, regular cheese) and meat (fatty beef, pork, lamb, poultry skin, bacon, bologna, salami, and pepperoni), saturated fats can increase blood cholesterol levels, leading to clogged arteries. High consumption of saturated fats may exacerbate inflammation, associated with arthritis, and trigger an overactive immune system, resulting in fatigue, joint pain, and blood vessel damage.
Fried Foods
Individuals with arthritis should avoid high-fat fried items such as fried chicken, French fries, donuts, and other deep-fried foods. Excessive consumption of fried foods contributes to increased body fat, adding stress to the joints. Some restaurants use hydrogenated oils (trans fats) for frying, further emphasizing the need for healthier cooking methods like grilling, steaming, roasting, and baking.
Refined Carbohydrates
Commonly found in foods made with white flour, such as white bread, rolls, crackers, and most baked goods, as well as white rice and certain cereals, refined carbohydrates lack the essential nutrients present in the bran and germ of whole grains. These carbohydrates promote inflammation in the body and worsen arthritis symptoms. Opt for healthier whole-grain alternatives like brown and wild rice, whole-wheat bread, whole-grain cereal, and whole-wheat pasta.
Simple Sugars
Present in fruit juice, soft drinks, candy, and cookies, simple sugars are refined carbohydrates that significantly elevate blood sugar levels, triggering an inflammatory response in the body. This escalation can exacerbate arthritis and its associated symptoms. Choose alternatives with lower sugar content to manage inflammation effectively.
- Sen R, Hurley JA. “Osteoarthritis.” [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482326.[↩]
- Bullock J, Rizvi SAA, Saleh AM, Ahmed SS, Do DP, Ansari RA, Ahmed J. “Rheumatoid Arthritis: A Brief Overview of the Treatment.” Med Princ Pract. 2018;27(6):501-507. doi: 10.1159/000493390. Epub 2018 Sep 2. PMID: 30173215; PMCID: PMC6422329.[↩]
- Ruschak I, Montesó-Curto P, Rosselló L, Aguilar Martín C, Sánchez-Montesó L, Toussaint L. “Fibromyalgia Syndrome Pain in Men and Women: A Scoping Review.” Healthcare (Basel). 2023 Jan 11;11(2):223. doi: 10.3390/healthcare11020223. PMID: 36673591; PMCID: PMC9859454.[↩]
- Cojocaru M, Cojocaru IM, Silosi I, Vrabie CD. “Manifestations of systemic lupus erythematosus.” Maedica (Bucur). 2011 Oct;6(4):330-6. PMID: 22879850; PMCID: PMC3391953.[↩]
- Kamen DL. “Environmental influences on systemic lupus erythematosus expression.” Rheum Dis Clin North Am. 2014 Aug;40(3):401-12, vii. doi: 10.1016/j.rdc.2014.05.003. PMID: 25034153; PMCID: PMC4198387.[↩]
- Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F; National Arthritis Data Workgroup. “Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II.” Arthritis Rheum. 2008 Jan;58(1):26-35. doi: 10.1002/art.23176. PMID: 18163497; PMCID: PMC3266664.[↩]
- Zhang Y, Jordan JM. “Epidemiology of osteoarthritis.” Clin Geriatr Med. 2010 Aug;26(3):355-69. doi: 10.1016/j.cger.2010.03.001. Erratum in: Clin Geriatr Med. 2013 May;29(2):ix. PMID: 20699159; PMCID: PMC2920533.[↩]
- Pal CP, Singh P, Chaturvedi S, Pruthi KK, Vij A. “Epidemiology of knee osteoarthritis in India and related factors.” Indian J Orthop. 2016 Sep;50(5):518-522. doi: 10.4103/0019-5413.189608. PMID: 27746495; PMCID: PMC5017174.[↩]
- Eakin GS, Amodeo KL, Kahlon RS. “Arthritis and its Public Health Burden.” Dela J Public Health. 2017 Mar 22;3(1):36-44. doi: 10.32481/djph.2017.03.006. PMID: 34466896; PMCID: PMC8352468.[↩]
- Fallon EA, Boring MA, Foster AL, Stowe EW, Lites TD, Odom EL, Seth P. “Prevalence of Diagnosed Arthritis – United States, 2019-2021.” MMWR Morb Mortal Wkly Rep. 2023 Oct 13;72(41):1101-1107. doi: 10.15585/mmwr.mm7241a1. PMID: 37824422; PMCID: PMC10578950.[↩]